Functional Hypothalamic Amenorrhoea (FHA) is a common reason for periods to stop after they have previously been regular. This is known as secondary amenorrhoea. FHA accounts for around 20–35% of all cases of secondary amenorrhoea.
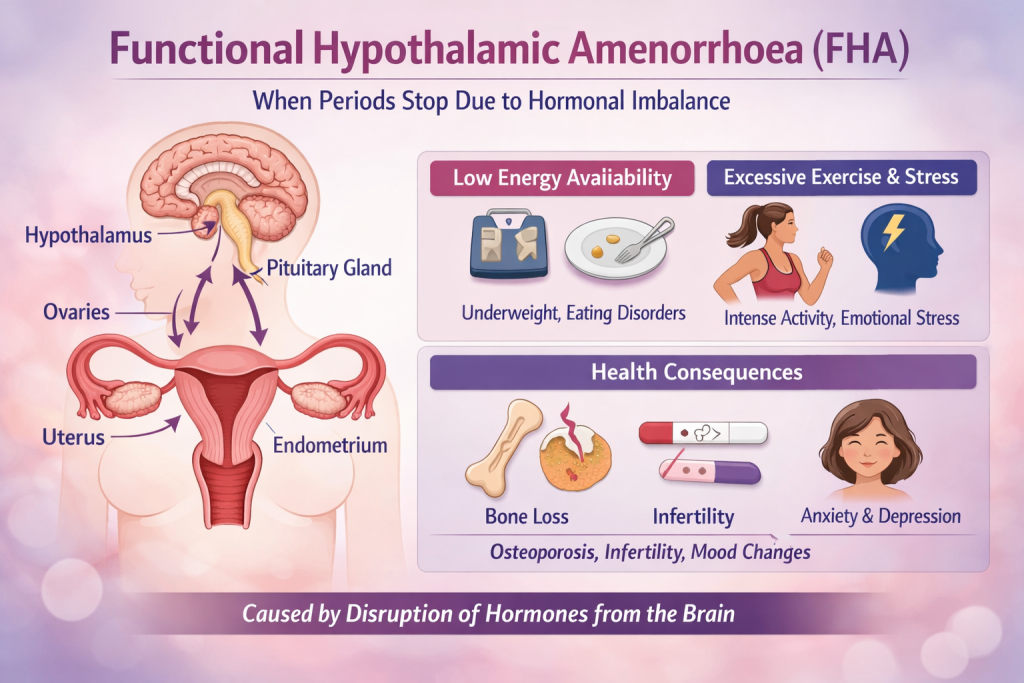
In a normal menstrual cycle, the brain (hypothalamus and pituitary gland), ovaries, and uterus work together in a carefully coordinated sequence each month. If pregnancy does not occur, this results in a menstrual bleed.
Periods can stop due to conditions affecting the hypothalamus, pituitary gland, ovaries, uterus, cervix, or vagina. In FHA, the hypothalamus reduces or stops releasing the hormones needed to stimulate the ovaries. As a result, the ovaries do not produce enough estrogen and progesterone, and the uterus is not stimulated to shed its lining—so periods stop.
FHA is commonly associated with:
- Low body weight or low body fat percentage
- Eating disorders
- Strenuous or excessive exercise
- Physical or emotional stress
- Certain medical conditions or illnesses
Why Does FHA Occur?
FHA usually develops due to a mismatch between energy intake and energy expenditure, leading to relative energy deficiency. Often, several factors are involved, and in some cases there may be no obvious trigger.
When your body does not have enough energy to meet its basic needs, it begins to shut down non-essential functions, including ovulation. This does not necessarily mean you have an eating disorder—it simply means your energy intake is lower than what your body currently requires.
Reduced Energy Availability
This may be due to:
Sudden weight loss
Eating disorders
Poor nutrient absorption (malabsorption), such as in gastrointestinal conditions where the body cannot properly absorb calories, protein, vitamins, or minerals
Increased Energy Use
This may be due to:
Strenuous or prolonged exercise
Extreme physical, nutritional, or emotional stress
Severe or chronic illness
Additional Contributing Factors
High metabolic states (e.g. severe infections, burns, traumatic injury, organ transplant)
Ongoing stress (work, study, relationships, or trauma), which increases cortisol and suppresses the hormonal pathway controlling the menstrual cycle
Genetic predisposition, making some individuals more susceptible than others
Common Signs and Symptoms
The most noticeable symptom is absence of periods for more than three months. Other symptoms may include:
Unintentional weight loss
Fatigue and low energy
Difficulty sleeping
Bone pain or fractures
Many of these symptoms occur because the ovaries are producing very low levels of estrogen.
Who Is Most at Risk?
FHA is more common in people who:
Have low body weight or eating disorders (e.g. anorexia nervosa)
Exercise excessively, especially in sports where leanness is emphasised (e.g. ballet, gymnastics, long-distance running)
Experience chronic or high levels of stress
How Is FHA Diagnosed?
FHA is diagnosed based on:
Your medical history
Physical examination
Blood tests
It is a diagnosis of exclusion, meaning other causes of missed periods must first be ruled out. There is no single test or scan that confirms FHA—rather, the diagnosis is made once other conditions have been excluded.
Health Effects Beyond Missed Periods
The absence of periods is often only the visible part of the problem. Most health effects are related to low estrogen levels.
Possible short- and long-term effects include:
Bone loss and increased fracture risk – Estrogen is essential for bone strength, especially in younger years
Fertility difficulties if periods do not return
Increased risk of anxiety and depression
Sleep problems, hair loss, and dry skin
Early diagnosis and treatment are important to reduce complications and protect long-term health. The impact depends on how long periods have been absent and the underlying cause.
Management and Treatment Options
The aim of treatment is to restore normal menstrual cycles and fertility by addressing the underlying cause.
This may include:
Improving nutrition and overall energy intake
Adjusting exercise levels to match nutritional intake
Stress management strategies such as mindfulness, yoga, or meditation
A multidisciplinary team may be involved, including a:
Dietitian
Exercise physiologist
Psychologist
Endocrinologist
Gynaecologist
What Is the Outlook?
FHA is usually reversible with timely and appropriate management. Once the underlying cause is corrected, periods and fertility can often return. However, there may be a delay between lifestyle changes and the return of normal cycles, so ongoing follow-up is important.
When to Seek Specialist Review
If you previously had regular periods and they have stopped for three months or more, please see your GP to arrange a referral to Dr Imran for further assessment.